Managing Incontinence After a Stroke

Key Takeaways
-
Up to 50% of stroke survivors experience incontinence.
-
Many regain some bladder/bowel control within one year.
-
Causes include muscle weakness, nerve damage, and mobility challenges.
-
Recovery strategies: bladder retraining, Kegels, biofeedback, pelvic floor stimulation.
-
Medical options may include medications, neuromodulation, or surgery.
-
A personalized plan with a healthcare provider is essential.
Every year in America, nearly 800,000 people suffer from a stroke, according to the Centers for Disease Control and Prevention (CDC), and almost half of stroke survivors experience incontinence as a result.
In observance of May as National Stroke Awareness Month, we want to provide more information about the link between strokes and incontinence, as well as management tips and treatment.
Most people who experience incontinence after a stroke will recover bladder and bowel control within a year, and this understanding can help with the transition, recovery and management both in the short term and for the future.
Stroke and Incontinence: Causes and Risk Factors
Not everyone who experiences a stroke develops incontinence as a result, but it does occur. The American Stroke Association reports that while urinary incontinence is most common after a stroke, bowel incontinence or constipation can become an issue as well.
There are a few reasons people may become incontinent after a stroke. Loss of bladder control or loss of bowel control after a stroke may occur due to:
-
Weakened muscles that control the bladder and bowel.
-
Inability for nerves to communicate (neurogenic bladder).
-
Unable to reach the bathroom in time (functional incontinence).
For those experiencing urinary incontinence after a stroke, there are a few different types. Check out the NorthShore article, “The Best Products for Different Types of Urinary Incontinence,” for details on stress and urge incontinence, overactive bladder and more.
Taking steps to manage incontinence, as well as understanding the products that can assist, can be helpful.
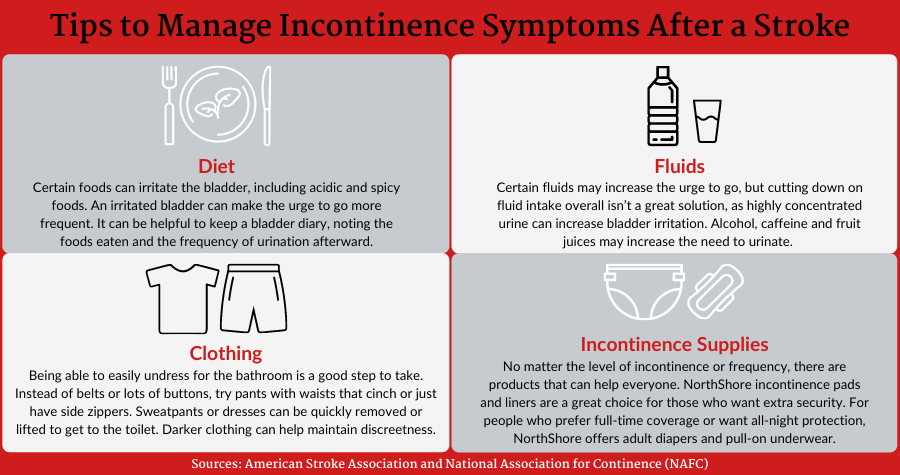
Tips to manage incontinence symptoms after a stroke
There are any number of adjustments people may need to make after experiencing a stroke. Someone may need a caregiver for the first time, especially in the days and weeks following, but a
high level of care may not be necessary for a long period of time. Rehabilitation could help people regain abilities lost.
People with incontinence and their caregivers can incorporate ways to manage incontinence after a stroke. A doctor or healthcare provider can provide information about what to expect as well. For those experiencing urinary incontinence for the first time, it can be helpful to take a look at the following:
Exercises and Therapies to Improve Bladder and Bowel Function After Stroke
Depending on the type of urinary incontinence you or your loved one is experiencing, there are a number of treatments and exercises available to help manage it. Remember, before starting any program, including exercise, discuss them with a doctor or healthcare provider. The National Association for Continence (NAFC) offers an informative overview of how to manage the various types of incontinence. Treatments include:
-
Bladder Retraining: This method involves scheduled voiding and urgency control through delayed urination, as well as Kegel exercises.
-
Biofeedback Training: This helps people identify the correct muscles to strengthen in their pelvic floor, and it can be done with a coach or with different products in the privacy of the home.
-
Pelvic Floor Stimulation: Strengthening these muscles can assist with urinary or bowel incontinence. Technology has advanced to the point that people can use electronic or magnetic stimulation.
-
Medical Procedures: Surgeries that create “slings” to assist with urinary incontinence are available.
-
Neuromodulation: This involves stimulating the sacral nerve to help treat stress or urge incontinence.
-
Medications: A doctor may recommend pharmaceutical treatments or discuss if current medications are causing urinary incontinence as a side effect.
Bladder Retraining Techniques for Post-Stroke Incontinence.
Both men and women can benefit from Kegel exercises, which help strengthen the pelvic floor muscles. Identify these muscles by imagining that you are stopping the flow of urine. Once those are isolated, practice strengthening them in three steps:
-
Contract the muscle for 3-5 seconds, then release for 3-5 seconds.
-
Work toward completing 10 repetitions a day.
-
As this gets easier, work toward holding and releasing for up to 10 seconds.
Remember to do Kegel exercises with an empty bladder. It can be helpful to perform these at set times of the day to make it a part of a routine. An effective schedule could be in the morning, at noon and in the evening after voiding.
Prompted voiding can also assist with urge incontinence, the sudden, overwhelming need to go with little warning. By scheduling bathroom breaks at regular intervals, people can help “retrain” their bladder. With some practice, people eventually can try to lengthen the time between scheduled bathroom breaks.
Practicing urgency control is another method to retrain the bladder. When the urge to go to the bathroom strikes, a person managing incontinence may take deep breaths, practice Kegels or count down from 100. Note that the goal isn’t to avoid the bathroom for too long, as that can cause issues such as urinary tract infections, but to practice building control over the immediate need to void.
Any or all of these incontinence exercises may help manage changes to the bowel or bladder after a stroke.
Here are a few other resources American Stroke Association provides:
Curious about all the NorthShore incontinence supplies that can help people live a full life while managing loss of bladder or bowel control? Visit the NorthShore Blog for more articles, advice, tips and guidance.
This article is not intended to substitute professional medical advice, diagnosis or treatment. Always speak to your doctor or other qualified healthcare provider with any questions or for advice regarding a medical condition.